Breast Pumping - a Learned Art of a Mother

Breast pumping is the process
of extracting milk out of woman's breasts with the help of a pump, as opposed to hand
expression when a mother removes milk from her breasts using hands.
Pumped breast milk can then be frozen and stored and thawed when needed.
Depending on your individual reason for pumping, your circumstances and behavior of your newborn baby, you may need to work out your personal pumping plan.
I am going to describe 6 most common scenarios. Mix and match as you need:
1. If your newborn is unable to latch or nurse for a while after the delivery
Start breast pumping as soon after the delivery as you physically can. You need to pump colostrum and give it to your baby. Colostrum is lifeblood for a newborn.
Use a good pump. A good pump can save you lots of time and nerves.
In general, if you plan to return to work after maternity leave, but
continue to breastfeed, you will need a good heavy-duty breast pump. If you get one now, you will be able to use it later too.
I used Medela Pump In Style Advanced and loved it. It is
very powerful and mimics baby's sucking. It also allows you to pump both breasts at the same time. It is perfect for building up the
supply and maintaining it until your baby is able to nurse. Learn more about this pump:
If you don’t have a pump, ask your hospital nurse if they rent pumps. Some hospitals do. Otherwise hand express milk. Don’t wait. Time is crucial.
If your baby still doesn’t nurse when your mature milk comes in, aim for 8-11 pumping sessions every 24 hours.
During the first 3-4 months of your baby’s life your breasts should be emptied every 2-3 hours. Unemptied breasts give your body a signal to produce less milk. And since this is the time when your supply is just getting established it is extremely important to keep your breasts well-drained.
If your first breast pumping happens while you are still in the hospital, take advantage of the hospital lactation consulting. Ask a lactation specialist to be present while you pump. You can learn some useful let-down techniques from them.
As your mature milk comes in, you should aim to pump 25-30 ounces of milk a day within a couple of weeks after the delivery. Your supply will grow gradually. Your baby will be eating up to 2 ounces every 2-3 hours. Extra milk should be frozen and saved in case of a non-productive day in the future. Visit Breast Milk Storage section to learn how to do that.
As your milk supply stabilizes, pump to empty your breasts completely, then hand express to get even more milk out.
Do not overdo it and exhaust yourself. Entire pumping session (if you are pumping both breasts simultaneously) shouldn’t last longer than 15 minutes. Your breasts need enough time to prepare for the next session.
But try not to leave any milk in your breasts after pumping. Even if your baby takes 2 ounces of milk at a time and you can pump 3, then pump 3.
Your baby’s demand will slightly grow with time. Since your baby doesn’t nurse, your body doesn't easily adjust to the increased demand. At times you may not be able to pump as much as needed. This is when your stored milk supply comes in handy.
To build up your milk supply, continue breast pumping for several minutes after milk stops flowing. This will give your body a signal to produce more.
When you reach the desired supply, smoothly decrease the number of times you pump. Take caution not to jeopardize your milk supply.
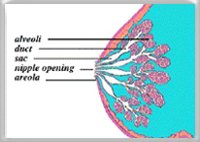
Remember: Your breast storage capacity is limited and it varies woman by woman. On average your body produces a minimum of 1 ounce of milk per hour by the end of the first month.
So let’s say your breast storage capacity (both
breasts) is 6 ounces, then it takes the maximum of 6 hours to use it up.
If you go longer than that without pumping, your milk-producing cells suppress production and your supply drops. Since it is hard to rely on an accurate estimation of your breasts’ capacity, it is safer to pump regularly.
Many babies refuse the breast after they are given a bottle. This phenomenon is called nipple confusion. To prevent nipple confusion try alternative methods of supplementing with your milk. Read about them here.
2. If you fully substitute breastfeeding with pumping from the very beginning for personal reasons or because your baby just won’t latch on
In this situation you'll be using your pump a lot, so you need a good pump.
Use guidelines from the previous section to build up your milk supply.
If your supply is dropping due to lack of breast stimulation and your baby refuses to latch because of your low milk supply, try using a Supplemental Nursing System.

SNS (Supplemental Nursing System) is a system consisting of a bottle and a thin tube. The tube is placed by the nipple.
When baby latches on the nipple, the tube is inserted in the corner of the baby’s mouth.
SNS is breastfeeding-friendly. The baby is sucking on the breast and gets rewarded by a steady milk flow from the tube.
3. If during first weeks of breastfeeding your baby latches on and nurses, but
doesn’t remove all the milk from the breasts due to weakness or health issues
Pump right after the feeding session to drain your breasts well. If advised
by the doctor, supplement your baby with your milk. Avoid bottles to prevent
nipple confusion.
Do not postpone pumping for too long after nursing. Your breasts need time to prepare for the next feeding.
4. If you breastfed exclusively, but now you need to return to work or be away from your baby
Choose a pump that corresponds your life style and your breast pumping
pattern. Medela Pump In Style worked perfectly for me when I went back to work. Click here to read the review.
Learn how your pump works and practice pumping before you really need to pump. It will make the learning curve stress-free and get you ready when you start depending on that pumped milk.
Ideally you should pump from the first days your milk supply becomes steady. You never know how your body will respond to pumping away from your baby. By the time you find out, you will have a freezer-full of pumped milk to feed your baby for weeks.
Pump shortly after first two feedings of the day. This is when the milk supply is the highest and your breasts are the fullest.
If you pump at work, but are unable to store milk and your baby is getting formula during the day, pump and dump to maintain supply.
5. If you pump to relieve breast or nipple condition
If you need to pump to relieve engorgement, mastitis, sore nipples, abscess, or clogged milk ducts, your goal is not collecting milk. So relax and disregard how much or little you pump.
You need to pump until the condition is relieved. Combine pumping with compresses and breast massage.
When the pain subsides and you are able to breastfeed – do so. Your baby is the most powerful "pumping machine".
Pump shortly before the feeding to relieve the fullness and help your baby latch on. Also pump after the feeding to remove any remaining milk to prevent further engorgement.
6. If you stopped breastfeeding and would like to start again (re-lactate) or you would like to breastfeed an adopted baby
Start breast pumping a couple of months before baby’s appearance (in case of adoptive breastfeeding).
When the baby is with you already, breastfeed. Baby’s sucking is the best stimulation for your breasts.
If there is still no milk in your breasts use a SNS (see above) to reward your baby’s nursing with milk or formula. You can get breast milk from a milk bank until your milk production starts.
Your doctor may prescribe hormones to stimulate milk production. They may include pregnancy hormones (for adopting mothers), which put your body through the simulated pregnancy, birth and the onset of mature milk.
This approach has to be started many months before the baby and may put you through all the pregnancy “pleasant” moments, like feeling sick and even gaining weight.
Once your milk starts (it may be clear in color at first), work up your milk supply. You can also try these traditional and non-traditional methods of boosting milk supply.
If your baby is reluctant to nurse, pump your milk and supplement.
Be patient and persevere. Avoid bottles and pacifiers at least till your baby learns how to nurse to prevent nipple confusion.
"Weaning" from Breast Pumping
When it’s time to stop breast pumping, stop gradually to avoid engorgement and duct clogging. Make sure you still have some stored milk just in case.
Morning pumping should be the last to go. This is when your breasts are the fullest and more milk is left behind.
Home › Breast Pumping